In a recent study published in the journal Nutrients, researchers in Australia reviewed the evidence on the Mediterranean diet (MD) and cardiovascular health outcomes in females.
Cardiovascular disease (CVD) is the primary cause of death among females worldwide. Nutrition plays a pivotal role in modifying cardiovascular risk factors and alleviating CVD risk. The MD is internationally the most recommended diet, characterized by high consumption of plant foods and mono-unsaturated fats, moderate fish, seafood, and dairy intake, and low red/processed meat intake. The present study reviewed the current knowledge on the impact of MD on CVD prevention in females.
Review: Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses
Cardioprotective benefits
Research suggests cardioprotective advantages due to the synergistic effects of the main food components in the MD. The MD is associated with improved lipid profile, blood pressure, vascular function, oxidative stress, and inflammatory markers. Studies suggest that the lipid-lowering effect of the MD might result from the (higher) intake of mono- and poly-unsaturated fats from plant foods and fish.
Increased consumption of phytosterols and fiber may also help in cholesterol absorption. Moreover, antioxidants, minerals, and flavonoids, which exert anti-inflammatory effects and decrease oxidative stress, are abundant in the MD. Besides, increased antioxidants may reduce reactive oxygen species while increasing the bioavailability of nitric oxide, thereby improving blood pressure and vascular function.
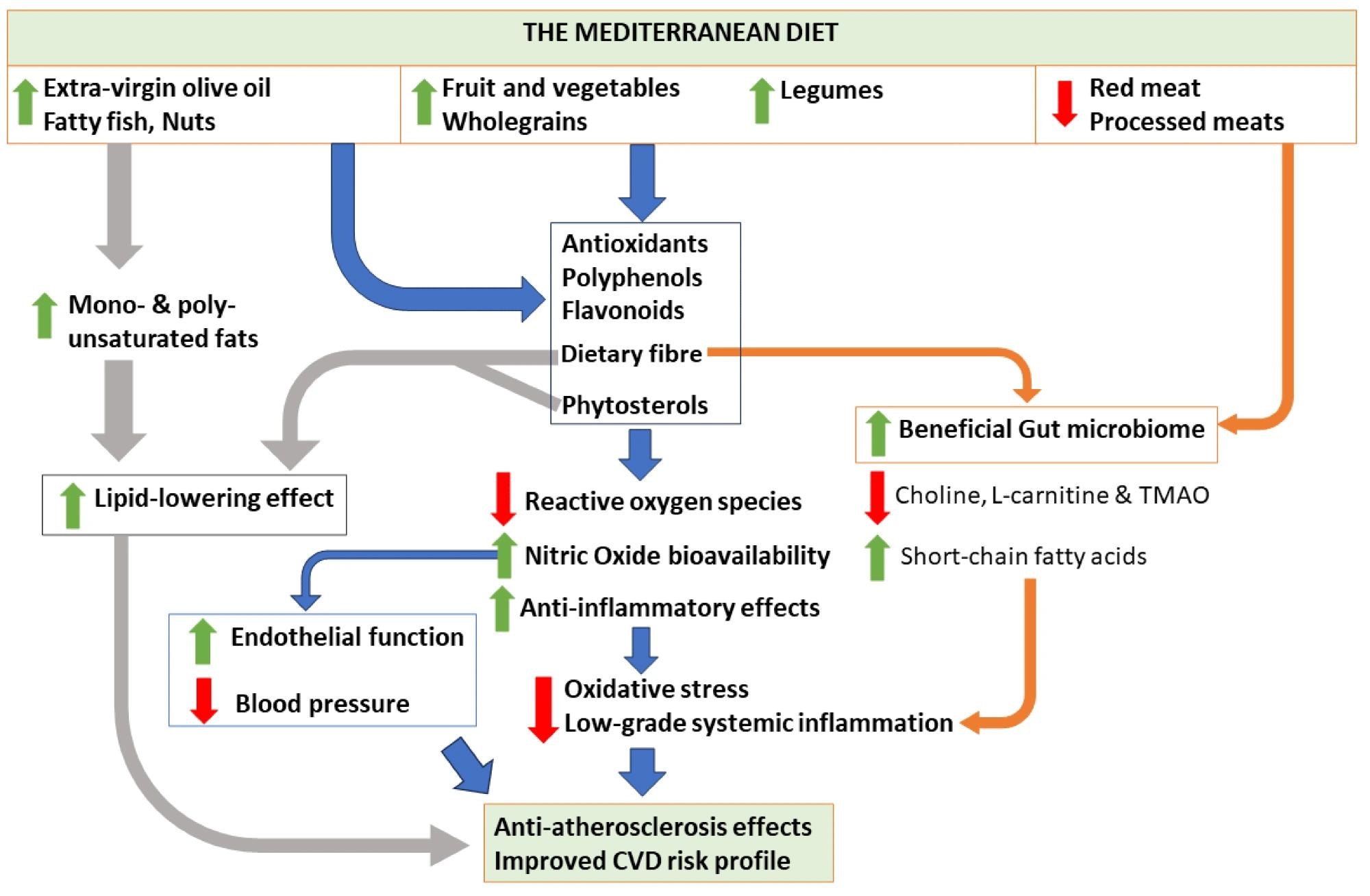 Possible mechanisms associated with the Mediterranean diet and its components, and their effects on cardiovascular health. TMAO, trimethylamine N-oxide; CVD, cardiovascular disease.
Possible mechanisms associated with the Mediterranean diet and its components, and their effects on cardiovascular health. TMAO, trimethylamine N-oxide; CVD, cardiovascular disease.
Sex-specific nutrition mechanisms
Biological sex is a significant factor in cardiovascular outcomes. The mechanistic interactions between the MD and sex remain unclear, with limited studies investigating this relationship. A pilot study revealed sex-dimorphic responses to the MD; specifically, MD-adherent females showed upregulation of apolipoprotein E and angiotensin-converting enzyme compared to males.
Animal studies have also reported sex differences in the gut microbiome, metabolism, and hormonal interactions. For instance, male mice fed a high-fat diet showed higher insulin resistance and weight gain, whereas females exhibited an increased abundance of beneficial microbes. Evolutionary pressures on dietary behavior, nutritional requirements, and physiology may explain the relationship between dietary patterns and sex.
Sex-dimorphic dietary behaviors have been common since the pre-Neolithic period. Females often gathered fruits/vegetables, while males hunted and consumed more high-fat foods and animal protein to meet energy demands. Thus, pre-historic gender roles may have modified the two sexes’ nutrient metabolism and energy requirements.
Current evidence on cardiovascular health
Studies have revealed lower risks of CVD with increased MD adherence. A large prospective cohort study of more than 74,000 females in the United States reported that greater MD adherence was associated with a 29% reduced risk of coronary heart disease. Some studies indicate that the MD has a more profound effect on CVD risk reduction in males than females, while others report significant effects in females only.
Various studies have demonstrated the beneficial effects of the MD on blood pressure. However, limited studies have focused on females. Further, the MD has been associated with a significantly lower risk of type 2 diabetes mellitus (T2DM) and improved glycated hemoglobin (HbA1c) and glucose levels.
In females, studies have reported benefits of the MD, including reduced T2DM incidence and improved insulin resistance and metabolic markers. In addition, a Canadian study reported that MD adherence was associated with lower body weight, body mass index (BMI), low-density lipoprotein cholesterol (LDL-C), and total cholesterol; notably, males had greater reductions in BMI and weight than females.
Female-specific risk factors
It is critical to have tailored treatment and prevention approaches for CVD and to reduce the burden in those with female-specific risk factors (pregnancy complications, polycystic ovarian syndrome [PCOS], and female-predominant autoimmune conditions). A trial in China involving 72 overweight patients with PCOS reported that a low-carbohydrate MD significantly reduced anthropometric and metabolic measures compared to a low-fat diet.
Numerous meta-analyses have revealed a nearly two-fold higher risk of future cardiovascular events in females with gestational diabetes mellitus, hypertensive disorders of pregnancy, or preterm birth. Nutritional supplementation and tailored dietary recommendations are associated with improved birth outcomes among females with poor nutrition. Short-chain poly-unsaturated fatty acids found in MD foods are essential during pregnancy.
Autoimmune conditions can occur at any age and have diverse manifestations. It is speculated that a genetic susceptibility to autoimmunity exists in females compared to males due to the X chromosome. Nevertheless, autoimmune disorders are linked to higher CVD risks in both sexes, but given the female preponderance, these conditions are likely more prevalent risk factors in females.
Conclusion
Together, current evidence supports the advantages of the MD in diverse populations, including females at high CVD risk. Nonetheless, future research on cardiovascular health requires higher female representation and sex-dimorphic and female-specific data. Further, additional studies are needed to determine whether the MD is more beneficial than other diets for female-specific conditions.
Journal reference:
- Pant A, Chew DP, Mamas MA, Zaman S. Cardiovascular Disease and the Mediterranean Diet: Insights into Sex-Specific Responses. Nutrients, 2024, DOI: 10.3390/nu16040570, https://www.mdpi.com/2072-6643/16/4/570
Credit: Source link




