- With both dementia and Alzheimer’s disease, early diagnosis is crucial to slow symptom progression.
- Because dementia and Alzheimer’s disease have the same or similar symptoms as age-related cognitive decline, they can be hard to diagnose at their earliest stages.
- Researchers from the University of Cambridge have developed an AI-based tool capable of predicting whether or not a person with early dementia symptoms will either remain stable or progress to Alzheimer’s disease.
While the terms dementia and Alzheimer’s disease are often used interchangeably, they are not the same.
With both dementia and Alzheimer’s disease, early diagnosis is key to help slow disease progression. However, previous studies show that
And because dementia and Alzheimer’s disease both share common symptoms of natural age-related cognitive decline, making early diagnosis of either condition is many times difficult.
In an effort to help solve this issue, researchers from the University of Cambridge have developed a tool using
The study was recently published in the journal
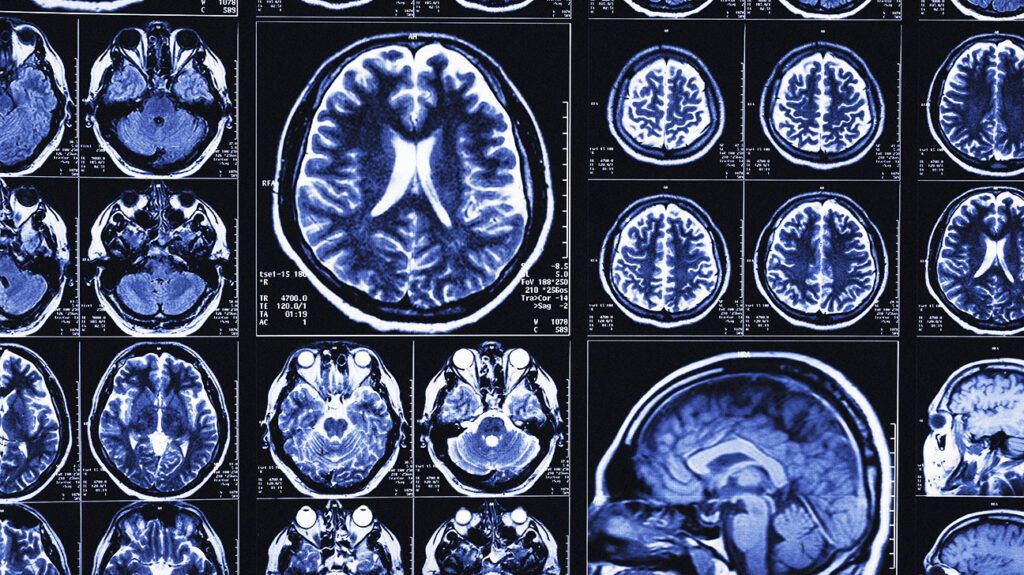
To build their AI tool, researchers used cognitive tests and MRI scan data from more than 400 people in a U.S.-based research group.
They then tested their AI tool on data from another 600 people in the U.S. research group, as well as 900 participants from memory clinics in the U.K. and Singapore.
“AI models are only as good as the data they are trained on,” explains Zoe Kourtzi, PhD, professor of experimental psychology and deputy head of research in the Department of Psychology at the University of Cambridge and senior author of this study.
“To make sure ours has the potential to be adopted in a healthcare setting, we trained and tested it on routinely collected data not just from research cohorts, but from patients in actual memory clinics. This shows it will be generalizable to a real-world setting,” she says.
According to researchers, the AI-based tool was able to tell the difference between study participants with fixed
All told, the tool was able to correctly spot 82% of participants who went on to develop Alzheimer’s disease and 81% of participants who did not based on MRI scans and cognitive tests alone.
Scientists said this made the AI tool almost three times more accurate at predicting progression from signs of early-stage dementia to Alzheimer’s disease than the current standard of care.
“We’ve created a tool which, despite using only data from cognitive tests and MRI scans, is much more sensitive than current approaches at predicting whether someone will progress from mild symptoms to Alzheimer’s — and if so, whether this progress will be fast or slow,” Kourtzi says.
“This [tool] has the potential to significantly improve patient well-being, showing us which people need closest care while removing the anxiety for those patients we predict will remain stable. At a time of intense pressure on healthcare resources, this will also help remove the need for unnecessary invasive and costly diagnostic tests.”
— Zoe Kourtzi, PhD
After reviewing this study, Manisha Parulekar, MD, FACP, AGSF, CMD, director of the Division of Geriatrics at Hackensack University Medical Center and co-director of the Center for Memory Loss and Brain Health at Hackensack University Medical Center in New Jersey, told Medical News Today that the development of an AI tool that can predict with 82% accuracy whether someone with early signs dementia will develop Alzheimer’s disease is a significant breakthrough.
“Currently, diagnosing Alzheimer’s disease in its early stages can be challenging. This information could be used to include lifestyle interventions, guide treatment decisions, and help patients and their families plan for the future.”
— Manisha Parulekar, MD, FACP, AGSF, CMD
“One of the challenges in research (has) been (the) inability to recruit patients with mild cognitive impairment in various treatment trials. This can also help identify patients with diverse backgrounds. Currently, most patients participating in trials are people with high health literacy. Early diagnosis allows patients to start treatment sooner, (and) recently approved medications are for patients with mild cognitive impairment and early Alzheimer’s dementia,” Parulekar added.
Parulekar said she would like to see this AI tool validated in a larger and more diverse population.
“The current study was conducted on a relatively small sample of patients,” she explained. “It is important to validate the tool in a larger and more diverse population to ensure that it is accurate and generalizable.”
MNT also spoke with David Merrill, MD, PhD, a geriatric psychiatrist and director of the Pacific Neuroscience Institute’s Pacific Brain Health Center at Providence Saint John’s Health Center in Santa Monica, CA, who commented that this study demonstrates the usefulness of AI to create accurate predictive models of dementia from information that is already commonly collected about patients in real-world care.
“Roughly half of patients with mild cognitive impairment don’t progress to dementia within five years, but half of patients do progress within five years and 10-15% progress within the first year after diagnosis. It’s important to accurately predict which patients need rapid and intensive intervention to prevent conversion into full-blown dementia versus those who may have more time or be at lower risk for conversion.”
— David Merrill, MD, PhD
“Use of this model and models like it may allow us to figure out what interventions result in true ‘rescues’ of preventing conversion in cases of patients who would have otherwise converted to dementia,” Merrill continued.
“Right now, it’s a 50-50 chance of a patient converting, so when there are anecdotal reports of ‘reversing’ dementia, are we really seeing cases not progress or is there reporting out of cases that were never going to progress to begin with? Demonstrating prevention of conversion of cases that were otherwise predicted to advance to dementia would be powerful evidence that an intervention is truly changing to (the) natural course of an individual’s disease course,” he said.
Credit: Source link